 Cleanzine: your weekly cleaning and hygiene industry newsletter 11th April 2024 Issue no. 1109
Cleanzine: your weekly cleaning and hygiene industry newsletter 11th April 2024 Issue no. 1109
Your industry news - first
The original and best - for over 20 years!
We strongly recommend viewing Cleanzine full size in your web browser. Click our masthead above to visit our website version.
HCAI quarterly trends January to March 2018, published
 Public Health England's latest quarterly commentary on trends in reports of Staphylococcus aureus (MRSA and MSSA) and Escherichia coli (E. coli) bacteraemia, and Clostridium difficile infections (CDI), mandatorily reported by NHS acute Trusts in England for the period January to March 2018, has been published and they show that there is still work to do when it comes to finding ways to prevent the spread of infection.
Public Health England's latest quarterly commentary on trends in reports of Staphylococcus aureus (MRSA and MSSA) and Escherichia coli (E. coli) bacteraemia, and Clostridium difficile infections (CDI), mandatorily reported by NHS acute Trusts in England for the period January to March 2018, has been published and they show that there is still work to do when it comes to finding ways to prevent the spread of infection.
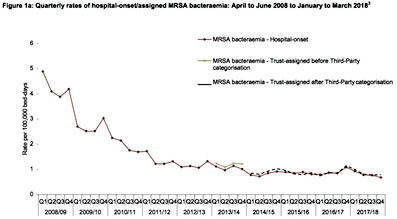
MRSA bacteraemia:
There had been a steep decline of 85% in the incidence rate (per 100,000 population) of all reported cases between April to June 2007 and January to March 2014 (from 10.2 to 1.5). This was followed by a 13% increase in incidence rates from 1.5 to 1.7 cases per 100,000 population between January to March 2014 and January to March 2018.
The Post-Implementation Review for all MRSA bacteraemia cases began in April 2013. Between April 2013 and March 2014, the incidence rate of trust-assigned cases remained stable at 1.2 cases per 100,000 bed days while the incidence rate of CCG-assigned cases decreased by 23% from 1.0 to 0.7 cases per 100,000 population.
Following the introduction of third-party assignment category in April 2014, incidence rates of CCG-assigned cases remained stable - at 0.7 cases per 100,000 population (n=91-92 cases) - between April to June 2014 and January to March 2018.
Over the same period (April to June 2014 to January to March 2018), incidence rates of the trust-assigned category remained relatively stable at 0.8 cases per 100,000 bed days (n=73-70) while counts and incidence rates of third-party assigned cases increased from 17 to 77 cases, and 0.1 to 0.6 per 100,000 population, respectively.
MSSA bacteraemia:
Since the mandatory reporting of MSSA bacteraemia began in January 2011, there has been a general trend of increasing counts and incidence rates. All reported cases increased by 38% from 2,199 to 3,037 between January to March 2011 and January to March 2018. This was accompanied by a 32% increase in incidence rate (per 100,000 population) from 16.8 to 22.1.
These increases are driven by community-onset cases. Over the same period (January 2011 to March 2018), counts and incidence rates of community-onset cases increased by 56% and 49% respectively - from 1,464 to 2,283 cases, and 11.2 to 16.6 cases per 100,000 population - while both counts and incidence rate of hospital-onset cases increased by 3% (735 to 754 cases), and 2% (8.4 to 8.5 cases per 100,000 bed-days), respectively.
When comparing the most recent quarter with the same period last year (January to March 2017 and January to March 2018), the incidence rate of hospital-onset MSSA bacteraemia decreased by 3% (from 8.8 to 8.5 cases per 100,000 bed-days) compared to a 3% increase in incidence rate of community-onset cases (from 16.2 to 16.6 cases per 100,000 population) over the same period.
Escherichia coli bacteraemia:
Seasonal peaks are seen in all reported cases of E. coli bacteraemia between July and September each year. Beginning April to June 2013, each quarter of each year has been higher than the same quarter in the preceding year, implying an increase over the overall time period. The seasonal peaks in all reported cases are due to the seasonality of community-onset cases.
Between July to September 2011 and January to March 2018, incidence rates of all reported cases increased by 12%, from 61.8 to 69.3 cases per 100,000 population (n = 8,275 - 9,519 cases). Similarly over the same period, incidence rates of community-onset cases increased by 19%, from 46.9 to 56.0 (n = 6,279 - 7,689 cases).
Unlike community-onset cases, between July to September 2011 and January to March 2018, hospital-onset cases decreased from 1,996 to 1,830 cases - corresponding to a 13% decrease in the associated incidence rate, from 23.7 to 20.7 per 100,000 bed-days.
Between January to March 2017 and January to March 2018 there was a 2% decrease in both counts and incidence rate of all reported cases: from 9,746 to 9,519 cases, and from 70.9 to 69.3 cases per 100,000 population, respectively. Compared to the fourth quarters of previous years, this is the first decrease since 2012 to 2013. Also both counts and the incidence rate of community-onset cases decreased by 2%, from 7,827 to 7,689 cases, and from 57.0 to 56.0 cases per 100,000 population, respectively.
Over the same period, the counts and incidence rate of hospital-onset cases decreased by 5%: from 1,919 to 1,830 cases, and from 21.7 to 20.7 cases per 100,000 bed-days, respectively.
Klebsiella spp. Bacteraemia:
In the first year of mandatory surveillance of Klebsiella spp. bacteraemia (2017 to 2018), a total of 9,617 cases of Klebsiella spp. bacteraemia were reported, an incidence rate of 17.4 cases per 100,000. During this time, 30% (n=2,853) were hospital-onset cases, an incidence rate of 8.2 cases per 100,000 bed-days. The remaining 70% (n=6,764) were community-onset cases, an incidence rate of 12.2 cases per 100,000 population.
Furthermore, over the same period, 68% (6,520/9,617) of all reported Klebsiella spp. bacteraemia were caused K. pneumoniae (the most frequently reported species) compared to 16% (1,497/9,617) caused by K. oxytoca (the next most frequently reported species).
Pseudomonas aeruginosa bacteraemia:
In the first year of mandatory surveillance (2017 to 2018), 4,286 cases of P. aeruginosabacteraemia have been reported with an incidence rate of 7.8 cases per 100,000 population. In 2017 to 2018, 38% (n=1,619) of cases were hospital-onset - an incidence rate of 4.7 cases per 100,000 bed-days; the remaining 62% (n=2,667) were community-onset cases - an incidence rate of 4.8 cases per 100,000 population.
Clostridium difficile infection:
Since the initiation of CDI surveillance in April 2007, there has been an overall decrease in counts and associated incidence rate of both all reported and hospital-onset cases of CDI. Seasonal peaks are present in January to March quarters prior to 2014 to 2015 and the July to September quarters between 2014 to 2015 and 2016 to 2017. This is particularly apparent among hospital-onset cases.
The bulk of this decrease occurred between April to June 2007 and January to March 2012 - with a 78% decrease in total (all reported) cases of CDI from 16,864 to 3,711 cases and an associated 79% reduction in incidence rate (per 100,000 population) from 131.6 to 27.9. Subsequently, between January to March 2012 and January to March 2018, all reported cases reduced by 17% - from 3,711 to 3,088 cases - and incidence rate reduced by 19% - from 27.9 and 22.5.
There were similar but greater reductions among hospital-onset CDI cases - an 85% reduction in cases, from 10,436 to 1,613, and an 84% reduction in incidence rate (per 100,000 bed days), from 112.5 to 18.2 - between April to June 2007 and January to March 2012. This was followed by a further 29% decrease in both counts (from 1,613 to 1,191 cases) and incidence rates (from 18.2 to 13.5 cases per 100,000 bed-days) - between January to March 2012 and January to March 2018. This shows that there has been a greater decline among hospital-onset CDI cases compared to all reported CDIcases during the surveillance period.
When the most recent quarter is compared with the same quarter last year (January to March 2017 and January to March 2018) both counts and incidence rate (per 100,000 population) of all reported CDI increased by 3% - from 2,990 to 3,088 cases and 21.8 to 22.5, respectively - while both counts and incidence rate (per 100,000 bed-days) of hospital-onset CDI cases both increased, slightly, by 8%: from 1,098 to 1,191 cases and 12.4 to 13.5 respectively.
28th June 2018







